It’s a Bad Time to Be a Booster Slacker
Americans aren’t getting the new bivalent COVID shot. What does that mean for the looming winter wave?
And just like that, with the passing of Labor Day, fall was upon us. Seemingly overnight, six-packs of pumpkin beer materialized on grocery shelves, hordes of city dwellers descended upon apple orchards—and America rolled out new COVID boosters. The timing wasn’t a coincidence. Since the beginning of the pandemic, cases in North America and Europe have risen during the fall and winter, and there was no reason to expect anything different this year. Spreading during colder weather is simply what respiratory diseases like COVID do. The hope for the fall booster rollout was that Americans would take it as an opportunity to supercharge their immunological defenses against the coronavirus in advance of a winter wave that we know is going to come.
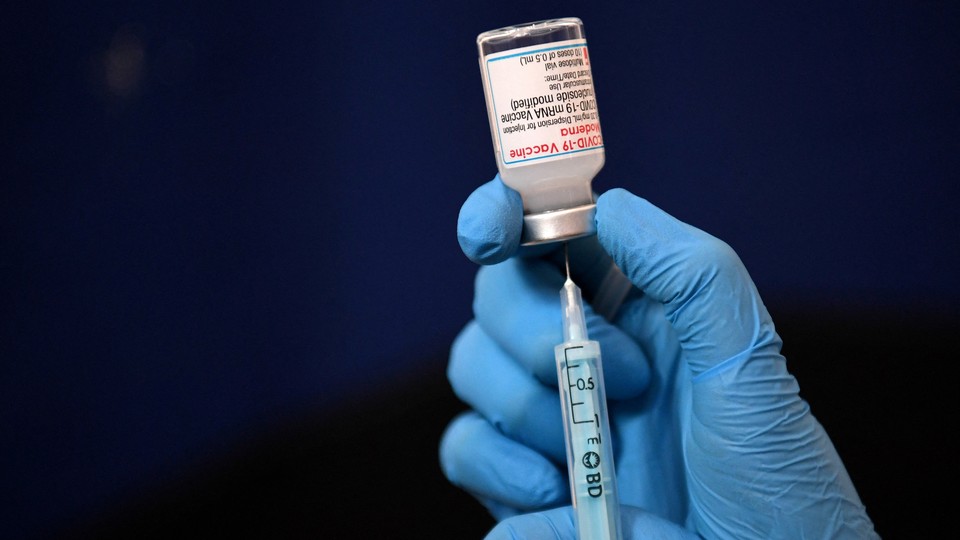
So far, reality isn’t living up to that hope. Since the new booster became available in early September, fewer than 20 million Americans have gotten the shot, according to the CDC—just 8.5 percent of those who are eligible. The White House COVID-19 response coordinator, Ashish Jha, said at a press conference earlier this month that he expects booster uptake to increase in October as the temperatures drop and people start taking winter diseases more seriously. That doesn’t seem to be happening yet. America’s booster campaign is going so badly that by late September, only half of Americans had heard even “some” information about the bivalent boosters, according to a recent survey. The low numbers are especially unfortunate because the remaining 91.5 percent of booster-eligible people have already shown that they’re open to vaccines by getting at least their first two shots—if not already at least one booster.
Now the bungled booster rollout could soon run headfirst into the winter wave. The virus is not yet surging in the United States—at least as far as we can tell—but as the weather cools down, cases have been on the rise in Western Europe, which has previously foreshadowed what happens in the U.S. At the same time, new Omicron offshoots such as BQ.1 and BQ.1.1 are gaining traction in the U.S., and others, including XBB, are creating problems in Singapore. Boosters are our best chance at protecting ourselves from getting swept up in whatever this virus throws at us next, but too few of us are getting them. What will happen if that doesn’t change?
The whole reason for new shots is that though the protection conferred by the original vaccines is tremendous, it has waned over time and with new variants. The latest booster, which is called “bivalent” because it targets both the original SARS-CoV-2 virus and BA.5, is meant to kick-start the production of more neutralizing antibodies, which in turn should prevent new infection in the short term, Katelyn Jetelina, a public-health expert who writes the newsletter Your Local Epidemiologist, told me. The other two goals for the vaccine are still being studied: The hope is that it will also broaden protection by teaching the immune system to recognize other aspects of the virus, and that it will make protection longer-lasting.
In theory, this souped-up booster would make a big difference heading into another wave. In September, a forecast presented by the Advisory Committee on Immunization Practices (ACIP), which advises the CDC, showed that if people get the bivalent booster at the same rate as they do the flu vaccine—optimistic, given that about 50 percent of people have gotten the flu vaccine in recent years—roughly 25 million infections, 1 million hospitalizations, and 100,000 deaths could be averted by the end of March 2023.
But these numbers shouldn’t be taken as gospel, because protection across the population varies widely and modeling can’t account for all of the nuance that happens in real life. Gaming out exactly what our dreadful booster rates mean going forward is not a simple endeavor “given that the immune landscape is becoming more and more complex,” Jetelina told me. People received their first shots and boosters at different times, if they got them at all. And the same is true of infections over the past year, with the added wrinkle that those who fell sick all didn’t get the same type of Omicron. All of these factors play a role in how much America’s immunological guardrails will hold up in the coming months. “But it’s very clear that a high booster rate would certainly help this winter,” Jetelina said.
At this point in the pandemic, getting COVID is far less daunting for healthy people than it was a year or two ago (although the prospect of developing long COVID still looms). The biggest concerns are hospitalizations and deaths, which make low booster uptake among vulnerable groups such as the elderly and immunocompromised especially worrying. That said, everyone ages 5 and up who has received their primary vaccine is encouraged to get the new booster. It bears repeating that vaccination not only protects against severe illness and death but has the secondary effect of preventing transmission, thereby reducing the chances of infecting the vulnerable.
What will happen next is hard to predict, Michael Osterholm, an epidemiologist at the University of Minnesota, told me, but now is a bad time for booster rates to be this low. Conditions are ripe for COVID’s spread. Protection is waning among the unboosted, immunity-dodging variants are emerging, and Americans just don’t seem to care about COVID anymore, Osterholm explained. The combination of these factors, he said, is “not a pretty picture.” By skipping boosters, people are missing out on the chance to offset these risks, though non-vaccine interventions such as masking and ventilation improvements can help too.
That’s not to say that the immunity conferred by vaccination and the initial boosters is moot. Earlier doses still offer “pretty substantial protection,” Saad Omer, a Yale epidemiologist, told me. Not only are eligible Americans slacking on booster uptake, but lately vaccine uptake among the unvaccinated hasn’t risen much either. Before the new bivalent shots came around, less than half of eligible Americans had gotten a booster. “That means we are, as a population, much more vulnerable going into this fall,” James Lawler, an infectious-diseases expert at the University of Nebraska Medical Center, told me.
If booster uptake—and vaccine uptake overall—remains low, expecting more illness, particularly among the vulnerable, would be reasonable, William Schaffner, a professor of infectious diseases at Vanderbilt University Medical Center, told me. Hospitalizations will rise more than they would otherwise, and with them the stress on the health-care system, which will also be grappling with the hundreds of thousands of people likely to be hospitalized for flu. While Omicron causes relatively minor symptoms, “it’s quite capable of producing severe disease,” Schaffner said. Since August, it has killed an average of 300 to 400 people each day.
All of this assumes that we won’t get a completely new variant, of course. So far, the BA.5 subvariant targeted by the bivalent booster is still dominating cases around the world. Newer ones, such as XBB, BQ.1.1, and BQ.1, are steadily gaining traction, but they’re still offshoots of Omicron. “We’re still very hopeful that the booster will be effective,” Jetelina said. But the odds of what she called an “Omicron-like event,” in which a completely new SARS-CoV-2 lineage—one that warrants a new Greek letter—emerges out of left field, are about 20 to 30 percent, she estimated. Even in this case, the bivalent nature of the booster would come in handy, helping protect against a wider crop of potential variants. The effectiveness of our shots against a brand-new variant depends on its mutations, and how much they overlap with those we’ve already seen, so “we’ll see,” Omer said.
Just as it isn’t too late to get boosted, there’s still time to improve uptake in advance of a wave. If you’re three to six months out from an infection or your last shot, the best thing you can do for your immune system right now is to get another dose, and do it soon. Though there’s no perfect and easy solution that can overcome widespread vaccine fatigue, that doesn’t mean trying isn’t worthwhile. “Right now, we don’t have a lot of people that feel the pandemic is that big of a problem,” and people are more likely to get vaccinated if they feel their health is challenged, Osterholm said.
There’s also plenty of room to crank the volume on the messaging in general: Not long ago, the initial vaccine campaign involved blasting social media with celebrity endorsers such as Dolly Parton and Olivia Rodrigo. Where is that now? Lots of pharmacies are swimming in vaccines, but making getting boosted even easier and more convenient can go a long way too. “We need to catch them where they come,” said Omer, who thinks boosters should be offered at workplaces, in churches and community centers, and at specialty clinics such as dialysis centers where patients are vulnerable by default.
After more than two years of covering and living through the pandemic, believe me: I get that people are over it. It’s easy not to care when the risks of COVID seem to be negligible. But while shedding masks is one thing, taking a blasé attitude toward boosters is another. Shots alone can’t solve all of our pandemic problems, but their unrivaled protective effects are fading. Without a re-up, when the winter wave reaches U.S. shores and more people start getting sick, the risks may no longer be so easy to ignore.